Background
Endovascular thrombectomy is a ground-breaking new treatment for severe stroke which requires specialist expertise and equipment. PenCHORD have collaborated with the Stroke Association, the National Institute for Health Research (NIHR) and NHS England in order to identify where and how this new service could be provided to maximise access to patients, and how it should interact with existing acute stroke services.
‘The modelling work undertaken by PenCHORD has been invaluable in helping the NHS decide how and where services for thrombectomy for stroke should be organised. It has also raised critical questions about the organisation of the whole of acute stroke care in way that will influence the new National Stroke Plan for England’
Professor Tony Rudd, National Clinical Director for Stroke, NHS England
Results showed that it is not possible for all current acute stroke units to provide and sustain the number of thrombectomy procedures required (at least 150 per year) to maintain an expert service. The maximum number of centres providing thrombectomy would be 40. It is therefore likely that a significant proportion of patients would require transfer from a local acute stroke unit to a comprehensive stroke unit providing thrombectomy, if they were judged suitable.
Modelling indicated that if ambulance crews started transferring patients directly to comprehensive stroke centres, local acute stroke services may be destabilised and comprehensive stroke centres may become overwhelmed. It was concluded that clear rules for ambulance crews will be required for effective roll-out of thrombectomy services.
Aims
The project aimed to determine:
- How many stroke units could provide a sustainable thrombectomy service, assuming that at least 150 procedures per year need to be carried out
- Where should these centres be located?
- Should patients be transferred directly to a comprehensive stroke centre providing thrombectomy if there was minimal effect on travel time (e.g. no more than 15 minutes extra travel time)?
Project activity
Modelling was based on the home location of 238,887 acute stroke patients admitted to hospital in England between 2013 and 2015. A bespoke ‘genetic algorithm’ was used to explore and optimise the number and choice of location of units potentially providing thrombectomy.
 Feasibility of a mothership model where all patients attend their closest comprehensive stroke centre providing thrombectomy.
Feasibility of a mothership model where all patients attend their closest comprehensive stroke centre providing thrombectomy.
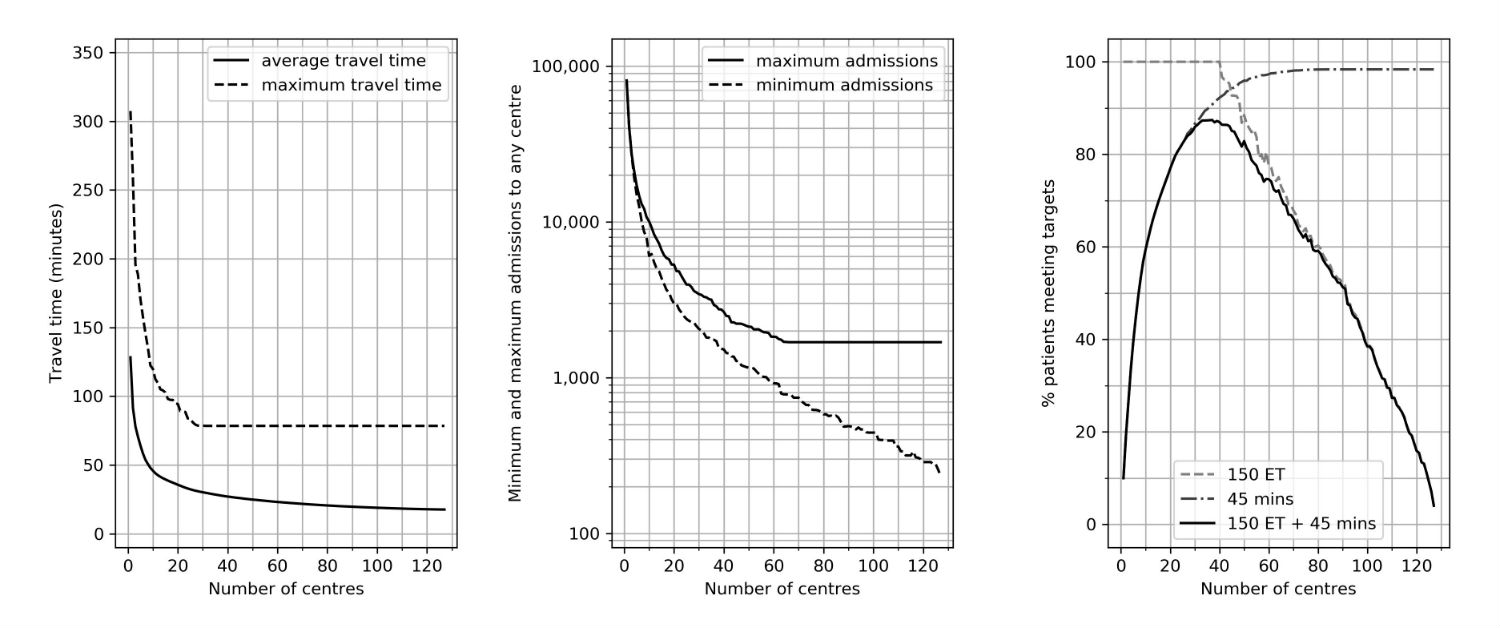
The panels show the relationship between the number of centres and best identified results for:
- (left panel) average and maximum travel time to centre
- (centre panel) greatest and fewest admissions per year to any single centre
- (right panel) the proportion of patients attending a centre within 45 minutes and providing at least 150 ET procedures per year
Outputs
Modelling results have been provided to the Stroke Association (who jointly funded the project with PenCLAHRC), NHS England, and the NIHR’s Promoting Effective and Rapid Stroke Care (PEARS) Project (which is looking at how best to implement thrombectomy services). This is now informing the review of roll-out of thrombectomy services in England.
Next Steps
PenCHORD are working with NHS England to define the next steps, likely to be more regional analysis of provision of thrombectomy services.
In the news
In July 2022 the Guardian ran a story about the low take-up of thrombectomy, citing the Stroke Association’s warning that ‘tens of thousands of patients to miss ‘gamechanging’ treatment unless NHS improves access.’
Stroke patients in England missing out on ‘miracle treatment’, warns report.
Related publications

Updating estimates of the number of UK stroke patients eligible for endovascular thrombectomy: incorporating recent evidence to facilitate service planning
Download the Paper
Mechanical thrombectomy for acute ischaemic stroke: an implementation guide for the UK - Second edition February 2022
Download the OtherThe cost of providing mechanical thrombectomy in the UK NHS: a micro-costing study
Download the PaperExploring the cost-effectiveness of mechanical thrombectomy beyond six hours following advanced imaging in the UK
Download the Paper
Mechanical thrombectomy for acute ischaemic stroke: an implementation guide for the UK - First edition August 2019
Download the OtherMaximising access to thrombectomy services for stroke in England: A modelling study
Download the PaperLinks and downloads
- Guardian news story July 2022 Stroke patients in England missing out on ‘miracle treatment’, warns report
Collaborators
- Stroke Association
PenARC Staff

Kerry Pearn
Research Fellow
Professor Martin James
Consultant Stroke Physician and Honorary Clinical Professor
